 |
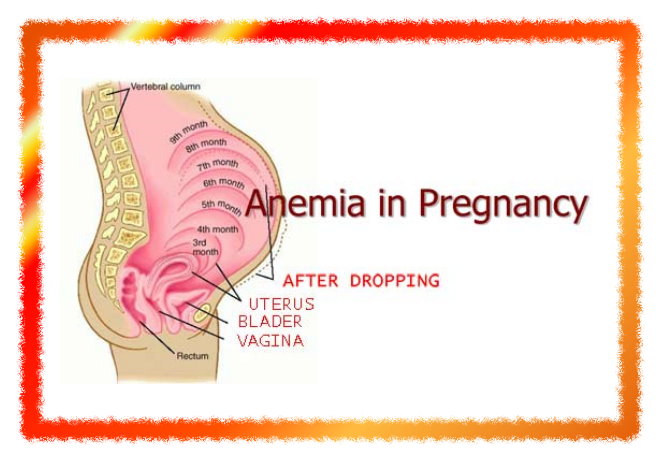
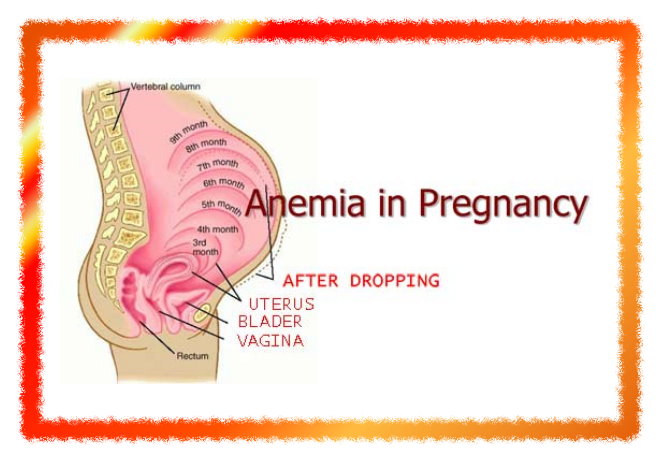
| Anaemia in pregnancy |
Anaemia in pregnancy
Classification of anamia:
1) physiological anaemia of prg.
2) pathological
A) iron deficiency anaemia
iron, folic acid, vit B 12 and protein def
B) haemorrhagic anaemia
a) acute - following bleedin in early months
b) chronic - hookworm infestation and
bleeding piles
C) heriditary
a) thalacemia
b) sickle cell anaemia
D) bone marrow insufficiancy
E) ananemia of infection
F) chr disease or neoplasm
Aetiology of iron deficiency anaemia
- low iron intake
- increase nutritional demand
- poor absorption and utilisation
- poor reserve
- increased loss of iron
C/F
A) symptoms
- fatigue, weakness, lassitude
- impaired work capacity
- dizziness, headache insomnia
- ankle oedema
- dyspnoea, palpitaion
- anorexia
B) signs
- pallar of skina nd mucus memb in severe
anaemia
- loss of palmer creases
- glossitis, dysphagia, stomatitis
- koilnychia
- tachycardia
Effect of anaemia on pregnancy
A) mother
1) during pregnancy
- cardia failure
- increase susseptibility of infection
- preterm labour
- pre-eclampsia
2) during labour
- uterina inertia
- PPH
- cardiac failure
- shock
3) during puerperium
- cardiac failure
- puerperial sepsis
- failing lactation
- chronic ill health, back ache
B) fetus and neonate
1) prematurity
2) IUGR and death
Investigations
A) for degree of anaemia
1) hb%
Mild 8-10 gm%
Moderate 7-8 gm%
Severe less than 7%
2) rbc count usually less tham 4 millions/ml
B) to know type of anaemia
1) peripheral smear
- to know marphology of RBC
- mocrocytic hypochromic
2) haematological indices
- MCH less than 25 pg
- PCV less than 30%
- MCHC less than 30%
- MCV less than 75 μmc
C) stool examination
- to detect parasitic inf
Like, ankylostoma, hookworm,
D) urine examination
- for presence of protein, sugar and pus cells
E) specific investigations
- vit B12 and folic acid in case of megaloblastic
anaemia
E) other blood values
- serum iron less than 30 μg/dl
- TIBC more than 400 μg/dl
- percentage saturaion 10% or less
- serum ferritin less than 15μg/lit
Treatment
(A) general prevention
- avoidance of frequent child births, minm interval shud b atleast 2 yrs
- supplimentary iron therapy- ferrus sulphate 200 mg (60 mg of elemental iron) with 1 mg of folic acid
- dietary prescription
Diet rich in iron and prtein like liver, vegitables, meat, eggs, jaggery
- fortification of food and salt by iron
- adequate rx of hookworm, bleeding piles, malaria, dysentru, UTI
- screening of adolescence girls in school
B) definative rx
1) iron therapy
a) oral iron therapy
- indicated in mild to mod anaemia
- 100-200 mg elemental iron per day
- common preparations r ferrous sulphate, ferrous fumarate, ferrous fumarate
- innitial dose- 200 mg ferrous sulphate thrice daily
- if large dose is required, shuld b raised gradulay in 3-4 days
- rx shuld b continued till blood picture bcomes normal
- thereafter maintainance dose of 1 tab daily for atleast 100 days following delivery to replenish iron stores
- side effects- nausea, vomiting, intolerance, diarrhoea, constipation, epigastric pain
b) parentaral iron therapy
Indications
- intolarance, noncompliace, poor absorption of oral therapy
Preparatio
- iron sorbitol citric acid complex
- iron dextran
Given im 100 mg/day on alternate day by Z technique
Side effects- painfull, abcess and staining at inj site
- intavenous route, required amt of iron (mg) =25 mg*percentage deficit
Complications r thrombophlebitis, fever and malise
Oral iron shuld be stopped b4 40 hr of parentaral iron
2) blood transfusion
- svr anaemia, svr haemorrhage ( aph, pph, cs), thalasemis, sickling dissorder
- by mak and sushil